The spring and summer of 2020 has brought many changes to all of our lives due to COVID-19. COVID-19 is a moving target; however, each day, we are getting one step closer to defeating it. We as Pediatricians daily get asked questions about COVID-19 as it relates to children.
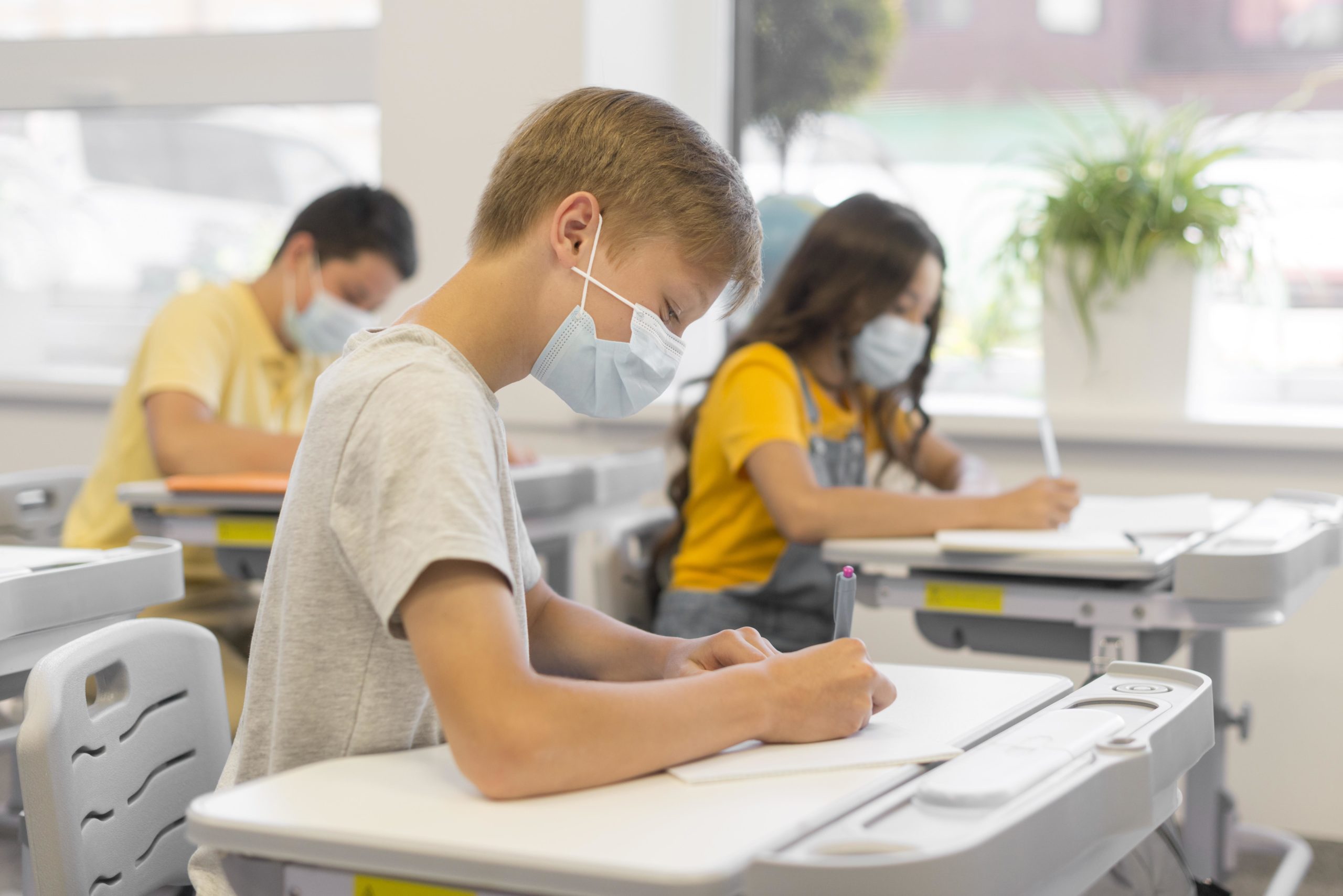
1. Should my children go to school in the Fall?
Yes, we believe that this Fall, children should return to school full-time (5 days per week) and
will be better off at school than trying to learn at home.
The American Academy of Pediatrics
has recently published several articles supporting the return to school this fall by helping the
schools establish guidelines to keep students, teachers, and staff members safe. Some of these
safety procedures may include wearing face masks, social distancing, grab and go lunches,
temperature checks, and frequent hand washing or hand sanitizer when entering classrooms.
There is a tremendous social and economic cost to closing schools, even partially. Parent,
including healthcare workers, can’t go to their jobs if they are home with children. Students are
likely to get a subpar education, with impacts on special needs students being potentially much
worse, as well as social isolation increasing and leading to increased mental health concerns
such as anxiety and depression.
We believe that the teachers should choose how best to protect themselves from potential
exposures, which may include, in addition to masks, face shields, outside teaching, spreading
desks out, or opening windows in classrooms (when temperatures cool down).
2. Should my child wear a face mask in public/at school?
Yes, we believe all children over the age of 2 should wear some form of face coverings while out
in public or at school.
Those 2 -5 year olds will have difficulty keeping masks in place, but
should still be encouraged to wear one. A cloth face covering over the nose and mouth is a safe
way to avoid spreading COVID-19. We also believe that all cloth masks should be washed daily.
3. How dangerous is COVID-19 to children?
The good news here is that MOST children who get COVID-19 do well with it. They may
experience a few days of fever, headaches, and some body aches—much like the symptoms of
the Flu.
The younger babies, under 10 weeks of age, are the ones at the highest risk, along
with any child with a chronic illness.
We at the Associates in Pediatric and Adolescent Medicine
(APAM), to date, have had NO admissions of COVID-19 positive children to the hospital and
have seen no deaths amongst our pediatric patients. The vast majority of the few COVID-19
positive patients we have seen are over 19 years old, with most only having a headache and/or
body aches, and some have had a cough.
4. What are your recommendations for kids/teen sports?
We recognize the vital importance that sports has in the overall development of children and
teens. As such we recommend a resumption of sports in the fall while taking as many
precautions as possible including further spacing during drills, frequent hand washing or using
hand sanitizer, not sharing water bottles, towels, gloves or bats, keeping players together in
smaller “pods” or groups to practice. We also recommend as much social distancing as
possible when off the field/court and discourage hand shaking, fist bumping, high fives or any
direct physical contact. We suggest that all coaches and spectators wear a mask and that off-
field/court players also mask up until they enter the game. Sports such as cross country, golf,
tennis and baseball are already set up to accommodate social distancing and should proceed
without interruption.
5. What are the rules about quarantine and testing if my child or I come in contact with a positive
COVID-19 person?
We, at APAM, follow the Center for Disease Control and Prevention (CDC) recommendations
that include NOT testing asymptomatic direct contact persons and NOT retesting previously
positive people unless they are returning to a nursing home or prison.
We do support 14 days
of home quarantine for significantly exposed persons, which include monitoring for symptoms
and frequent temperature checks at least twice a day for fever. If at any time during the 14 days,
any symptoms develop, the person should contact us and discuss whether to be tested.
We
also strongly support social distancing, which will undoubtedly decrease a person’s overall risk
of coming into contact with a COVID positive person.
<a href=”https://www.freepik.com/free-photos-vectors/school”>School photo created by freepik – www.freepik.com</a>
